Techniques To Care For Pes Planus
Overview
Rigid fallen arches are usually easy to distinguish from the flexible variety by the pain the cause, but there is a simple test that a person can perform if he is not sure. He should stand on the toes, and if the arch appears, the condition is known as flexible flat foot and is nothing to worry about. There have been Olympic runners with flat feet of this kind. On the other hand, if the foot remains flat on the bottom when the person stands on his toes, the condition is rigid, and the individual should consult a podiatrist. The same is true if a person notices any change in the arches of his feet or if he as foot pain, whether or not this test suggests he has flexible flat feet.
Causes
Flat feet are often a congenital problem which has no specific cause. They can however occur after an injury, especially conditions such as Tibialis Posterior Syndrome or more traumatic injuries such as fractures or mid-tarsal joint sprains. The other thing to look out for is Overpronation. Often this is confused with having flat feet (or a fallen arch) although it is not technically the same thing. If an individual does not have flat feet but does overpronate then the arch of their foot appears to be normal when standing. However, when they walk the arch collapses and the foot rolls in excessively. This is more difficult to spot than flat feet. It is estimated that between 60 and 80% of the population overpronate!
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
pes planus orthotics
Non Surgical Treatment
Switch activities for a little while. If you?re a super athlete, you don?t want to hear that you need to take a break, but there?s no way around it. You need to lay off the high impact sports like basketball, tennis and running. Don?t panic-there?s no shortage of alternatives. Find a high school track that?s open to the public and try going for a run. Many athletic programs use spongy synthetic materials to pave tracks instead of concrete. This is much easier on all the joints and tendons, not only in your feet but your legs and ankles. You can also try running on dirt trails or stable grassy areas. Take up swimming for a little while. This is actually an ideal activity for your arches. The buoyancy of water takes weight off our feet, but still allows for aerobic activity. Many gyms and activity centers also offer various water sport classes. In no time flat, you?ll be on your way to healthier feet.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Rigid fallen arches are usually easy to distinguish from the flexible variety by the pain the cause, but there is a simple test that a person can perform if he is not sure. He should stand on the toes, and if the arch appears, the condition is known as flexible flat foot and is nothing to worry about. There have been Olympic runners with flat feet of this kind. On the other hand, if the foot remains flat on the bottom when the person stands on his toes, the condition is rigid, and the individual should consult a podiatrist. The same is true if a person notices any change in the arches of his feet or if he as foot pain, whether or not this test suggests he has flexible flat feet.
Causes
Flat feet are often a congenital problem which has no specific cause. They can however occur after an injury, especially conditions such as Tibialis Posterior Syndrome or more traumatic injuries such as fractures or mid-tarsal joint sprains. The other thing to look out for is Overpronation. Often this is confused with having flat feet (or a fallen arch) although it is not technically the same thing. If an individual does not have flat feet but does overpronate then the arch of their foot appears to be normal when standing. However, when they walk the arch collapses and the foot rolls in excessively. This is more difficult to spot than flat feet. It is estimated that between 60 and 80% of the population overpronate!
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
pes planus orthotics
Non Surgical Treatment
Switch activities for a little while. If you?re a super athlete, you don?t want to hear that you need to take a break, but there?s no way around it. You need to lay off the high impact sports like basketball, tennis and running. Don?t panic-there?s no shortage of alternatives. Find a high school track that?s open to the public and try going for a run. Many athletic programs use spongy synthetic materials to pave tracks instead of concrete. This is much easier on all the joints and tendons, not only in your feet but your legs and ankles. You can also try running on dirt trails or stable grassy areas. Take up swimming for a little while. This is actually an ideal activity for your arches. The buoyancy of water takes weight off our feet, but still allows for aerobic activity. Many gyms and activity centers also offer various water sport classes. In no time flat, you?ll be on your way to healthier feet.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Limb Length Discrepancy Exercise
Overview
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.
Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
A qualified musculoskeletal expert will first take a medical history and conduct a physical exam. Other tests may include X-rays, MRI, or CT scan to diagnose the root cause.
Non Surgical Treatment
People with uneven leg lengths may be more prone to pain in their back, hips, and knees; uneven gait; and lower leg and foot problems. Due to its risks, surgery is typically not recommended unless the difference is greater than one inch. In cases where the difference is less than one inch, providing the same support for both feet is the most effective. This can be achieved by getting custom-fitted orthotics for both feet. Orthotics are inserts that you wear in the shoes. Your chiropractor will request to measure your feet and possibly your legs. You can step on a device that will take the measurements or you might have a plaster cast of your feet taken. Orthotics are typically made from plastic and leather, and function biomechanically with your foot. If a leg length discrepancy is not properly corrected with orthotics, your chiropractor may recommend a heel lift, also known as a shoe lift. You simply place it in the back of your shoe along with the orthotic. Typically, you will only wear the heel lift in one shoe to assist the shorter leg.

height increase food
Surgical Treatment
Limb deformity or leg length problems can be treated by applying an external frame to the leg. The frame consists of metal rings which go round the limb. The rings are held onto the body by wires and metal pins which pass through the skin and are anchored into the bone. During this operation, the bone is divided. Gradual adjustment of the frame results in creation of a new bone allowing a limb to be lengthened. The procedure involves the child having an anaesthetic. The child is normally in hospital for one week. The child and family are encouraged to clean pin sites around the limb. The adjustments of the frame (distractions) are performed by the child and/or family. The child is normally encouraged to walk on the operated limb and to actively exercise the joints above and below the frame. The child is normally reviewed on a weekly basis in clinic to monitor the correction of the deformity. The frame normally remains in place for 3 months up to one year depending on the condition which is being treated. The frame is normally removed under a general anaesthetic at the end of treatment.
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.

Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
A qualified musculoskeletal expert will first take a medical history and conduct a physical exam. Other tests may include X-rays, MRI, or CT scan to diagnose the root cause.
Non Surgical Treatment
People with uneven leg lengths may be more prone to pain in their back, hips, and knees; uneven gait; and lower leg and foot problems. Due to its risks, surgery is typically not recommended unless the difference is greater than one inch. In cases where the difference is less than one inch, providing the same support for both feet is the most effective. This can be achieved by getting custom-fitted orthotics for both feet. Orthotics are inserts that you wear in the shoes. Your chiropractor will request to measure your feet and possibly your legs. You can step on a device that will take the measurements or you might have a plaster cast of your feet taken. Orthotics are typically made from plastic and leather, and function biomechanically with your foot. If a leg length discrepancy is not properly corrected with orthotics, your chiropractor may recommend a heel lift, also known as a shoe lift. You simply place it in the back of your shoe along with the orthotic. Typically, you will only wear the heel lift in one shoe to assist the shorter leg.

height increase food
Surgical Treatment
Limb deformity or leg length problems can be treated by applying an external frame to the leg. The frame consists of metal rings which go round the limb. The rings are held onto the body by wires and metal pins which pass through the skin and are anchored into the bone. During this operation, the bone is divided. Gradual adjustment of the frame results in creation of a new bone allowing a limb to be lengthened. The procedure involves the child having an anaesthetic. The child is normally in hospital for one week. The child and family are encouraged to clean pin sites around the limb. The adjustments of the frame (distractions) are performed by the child and/or family. The child is normally encouraged to walk on the operated limb and to actively exercise the joints above and below the frame. The child is normally reviewed on a weekly basis in clinic to monitor the correction of the deformity. The frame normally remains in place for 3 months up to one year depending on the condition which is being treated. The frame is normally removed under a general anaesthetic at the end of treatment.
Understanding Heel Aches
Overview

Every mile you walk puts tons of stress on each foot. Your feet can handle a heavy load, but too much stress pushes them over their limits. When you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues, you may develop heel pain, the most common problem affecting the foot and ankle. A sore heel will usually get better on its own without surgery if you give it enough rest. However, many people ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to walk on a sore heel, it will only get worse and could become a chronic condition leading to more problems.
Causes
Age plays a large role in the development of heel pain, particularly among those over 40. Being active is also a common factor of heel pain. Over time, the elasticity of the tissue in our feet decreases with age, causing us to become prone to damage and also slowing the body's ability to heal damage. Adolescents are also not immune to heel pain. Those who are active in sports are particularly prone to excessively stretching or straining the plantar fascia or Achilles tendon, causing severe heel pain. In most cases, heel pain develops in only one heel. There are many risk factors that lead to heel pain. Abnormal gait and excessive, repetitive stress are common factors in the development of pain and damage. Among the other risk factors involved with the development of heel pain are repetitive exercise or activities, such as long distance running or jumping from activities such as basketball. Obesity. Walking barefoot on hard surfaces. Prolonged standing. Wearing poor fitting shoes, or shoes that do not provide enough support or cushioning. Not stretching properly or at all before and after exercise. Those who are on their feet for long periods of time.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
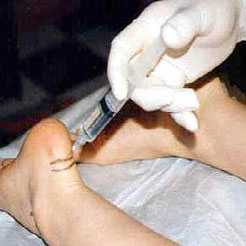
If pain and other symptoms of inflammation-redness, swelling, heat-persist, you should limit normal daily activities and contact our office, or another doctor of podiatric medicine. Your foot would be examined, and an X-ray may be taken to rule out problems of the bone. Early treatment might involve oral or injectable anti-inflammatory medication, taping, padding, massage, stretching, exercise, shoe recommendations, physiotherapy, over-the-counter shoe inserts or, if the condition is chronic and there is a biomechanical basis to the complaint, orthoses (or orthotic devices) may be used to permanently take strain off the fascia. Only rarely is surgery required for heel pain. If necessary, however, it may involve the release of the plantar fascia, removal of a spur, removal of a bursa, or removal of a neuroma or other soft-tissue growth.
Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints or a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as open surgery, where the section of the plantar fascia is released by making a cut into your heel or endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team.
heel pain exercises
Prevention

You can try to avoid the things that cause heel pain to start avoid becoming overweight, where your job allows, minimise the shock to your feet from constant pounding on hard surfaces, reduce the shocks on your heel by choosing footwear with some padding or shock-absorbing material in the heel, if you have high-arched feet or flat feet a moulded insole in your shoe may reduce the stresses on your feet, if you have an injury to your ankle or foot, make sure you exercise afterwards to get back as much movement as possible to reduce the stresses on your foot and your heel in particular, If you start to get heel pain, doing the above things may enable the natural healing process to get underway and the pain to improve.

Every mile you walk puts tons of stress on each foot. Your feet can handle a heavy load, but too much stress pushes them over their limits. When you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues, you may develop heel pain, the most common problem affecting the foot and ankle. A sore heel will usually get better on its own without surgery if you give it enough rest. However, many people ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to walk on a sore heel, it will only get worse and could become a chronic condition leading to more problems.
Causes
Age plays a large role in the development of heel pain, particularly among those over 40. Being active is also a common factor of heel pain. Over time, the elasticity of the tissue in our feet decreases with age, causing us to become prone to damage and also slowing the body's ability to heal damage. Adolescents are also not immune to heel pain. Those who are active in sports are particularly prone to excessively stretching or straining the plantar fascia or Achilles tendon, causing severe heel pain. In most cases, heel pain develops in only one heel. There are many risk factors that lead to heel pain. Abnormal gait and excessive, repetitive stress are common factors in the development of pain and damage. Among the other risk factors involved with the development of heel pain are repetitive exercise or activities, such as long distance running or jumping from activities such as basketball. Obesity. Walking barefoot on hard surfaces. Prolonged standing. Wearing poor fitting shoes, or shoes that do not provide enough support or cushioning. Not stretching properly or at all before and after exercise. Those who are on their feet for long periods of time.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
If pain and other symptoms of inflammation-redness, swelling, heat-persist, you should limit normal daily activities and contact our office, or another doctor of podiatric medicine. Your foot would be examined, and an X-ray may be taken to rule out problems of the bone. Early treatment might involve oral or injectable anti-inflammatory medication, taping, padding, massage, stretching, exercise, shoe recommendations, physiotherapy, over-the-counter shoe inserts or, if the condition is chronic and there is a biomechanical basis to the complaint, orthoses (or orthotic devices) may be used to permanently take strain off the fascia. Only rarely is surgery required for heel pain. If necessary, however, it may involve the release of the plantar fascia, removal of a spur, removal of a bursa, or removal of a neuroma or other soft-tissue growth.
Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints or a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as open surgery, where the section of the plantar fascia is released by making a cut into your heel or endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team.
heel pain exercises
Prevention

You can try to avoid the things that cause heel pain to start avoid becoming overweight, where your job allows, minimise the shock to your feet from constant pounding on hard surfaces, reduce the shocks on your heel by choosing footwear with some padding or shock-absorbing material in the heel, if you have high-arched feet or flat feet a moulded insole in your shoe may reduce the stresses on your feet, if you have an injury to your ankle or foot, make sure you exercise afterwards to get back as much movement as possible to reduce the stresses on your foot and your heel in particular, If you start to get heel pain, doing the above things may enable the natural healing process to get underway and the pain to improve.
Treating Mortons Neuroma
Overview
 Morton?s Neuroma is a pain condition that affects your feet and toes. If you are suffering from Morton?s Neuroma, a growth of tissue has developed over one of the nerves running from your feet into your toes. This growth can cause inflammation and pain whenever you use your foot. A type of benign tumor, Morton?s Neuroma typically develops in the space between the third and fourth toes, although it can also form between the second and third toes. When you walk, the bones and ligaments in the top of your foot press down on this growth, causing pressure and pain.
Morton?s Neuroma is a pain condition that affects your feet and toes. If you are suffering from Morton?s Neuroma, a growth of tissue has developed over one of the nerves running from your feet into your toes. This growth can cause inflammation and pain whenever you use your foot. A type of benign tumor, Morton?s Neuroma typically develops in the space between the third and fourth toes, although it can also form between the second and third toes. When you walk, the bones and ligaments in the top of your foot press down on this growth, causing pressure and pain.
Causes
Although in many areas of medicine, it?s easy to pinpoint the exact source of a problem (the way a specific germ causes a certain illness with recognizable symptoms), neuromas are harder to categorize. While there isn?t really one exact cause, podiatric physicians tend to agree that a neuroma can occur in response to the irritation of a nerve by one or more factors. Abnormality in foot function or foot mechanics: In other words, a foot that doesn?t move the way science thinks it should. In general, this means a pronated foot (one with an excessive rolling motion when the patient is walking, running or doing any kind of activity), because it causes excessive strain on the nerve. If you are not certain whether or not this is a problem for you, ask your podiatric physician, who will be able to examine your feet, as well as the wear pattern on your shoe, and give you an answer. Foot mechanics, and problems with them, tend to run in families, so if you know that a relative has had foot pain similar to yours, be sure to mention it.
Symptoms
You may initially experience a tingling sensation in the space between your toes, which gets worse over time. This leads to cramp in your toes and a sharp shooting or burning pain on the ball of your foot or at the base of your toes. The pain is often worse when walking or wearing shoes that press on the affected area. This is caused by irritation of the nerve between your toe bones (metatarsal bones). The tingling will eventually lead to pain, which can get worse over time. You may also experience cramping of your toes. The pain is usually felt as a sharp shooting or burning pain on the ball of the foot or at the base of the toes, which is often made worse when you're walking. Some people with Morton's neuroma feel anxious about walking or even placing their foot on the ground. The pain is likely to be more intense if you wear tight shoes, so wearing shoes that have more room in the toe area can help. Rubbing your foot may also lessen the pain.
Diagnosis
The exact cause of Mortons neuroma can often vary between patients. An accurate diagnosis must be carefully made by the podiatrist through thorough history taking and direct questioning to ensure all possible causes are addressed. The podiatrist will also gather further information about the cause through a hands on assessment where they will try to reproduce your symptoms. A biomechanical and gait analysis will also be performed to assess whether poor foot alignment and function has contributed to your neuroma.
Non Surgical Treatment
It can be helpful to perform deep stripping massage techniques along the length of the tibial nerve and the medial and lateral plantar nerves. After properly mobilizing these tissues, moving the foot and toes through a full range of motion to make sure the nerve can move freely will also be helpful. Foot pain like that occurring in Morton's neuroma, can become a debilitating and painful condition. And while massage can be helpful for this condition, it is also clear that improperly applied massage can aggravate it and make it worse. Consequently it is crucial that we use good clinical reasoning and appropriate evaluation methods to most effectively help these clients.
Surgical Treatment
If your pain continues despite several months of conservative treatment, your doctor may recommend surgery to remove the neuroma or to widen the space through which the affected nerve travels. These types of surgery often are done under local anesthesia. If your doctor removes a portion of the affected nerve along with the neuroma, you may develop permanent numbness between the toes.
 Morton?s Neuroma is a pain condition that affects your feet and toes. If you are suffering from Morton?s Neuroma, a growth of tissue has developed over one of the nerves running from your feet into your toes. This growth can cause inflammation and pain whenever you use your foot. A type of benign tumor, Morton?s Neuroma typically develops in the space between the third and fourth toes, although it can also form between the second and third toes. When you walk, the bones and ligaments in the top of your foot press down on this growth, causing pressure and pain.
Morton?s Neuroma is a pain condition that affects your feet and toes. If you are suffering from Morton?s Neuroma, a growth of tissue has developed over one of the nerves running from your feet into your toes. This growth can cause inflammation and pain whenever you use your foot. A type of benign tumor, Morton?s Neuroma typically develops in the space between the third and fourth toes, although it can also form between the second and third toes. When you walk, the bones and ligaments in the top of your foot press down on this growth, causing pressure and pain.Causes
Although in many areas of medicine, it?s easy to pinpoint the exact source of a problem (the way a specific germ causes a certain illness with recognizable symptoms), neuromas are harder to categorize. While there isn?t really one exact cause, podiatric physicians tend to agree that a neuroma can occur in response to the irritation of a nerve by one or more factors. Abnormality in foot function or foot mechanics: In other words, a foot that doesn?t move the way science thinks it should. In general, this means a pronated foot (one with an excessive rolling motion when the patient is walking, running or doing any kind of activity), because it causes excessive strain on the nerve. If you are not certain whether or not this is a problem for you, ask your podiatric physician, who will be able to examine your feet, as well as the wear pattern on your shoe, and give you an answer. Foot mechanics, and problems with them, tend to run in families, so if you know that a relative has had foot pain similar to yours, be sure to mention it.
Symptoms
You may initially experience a tingling sensation in the space between your toes, which gets worse over time. This leads to cramp in your toes and a sharp shooting or burning pain on the ball of your foot or at the base of your toes. The pain is often worse when walking or wearing shoes that press on the affected area. This is caused by irritation of the nerve between your toe bones (metatarsal bones). The tingling will eventually lead to pain, which can get worse over time. You may also experience cramping of your toes. The pain is usually felt as a sharp shooting or burning pain on the ball of the foot or at the base of the toes, which is often made worse when you're walking. Some people with Morton's neuroma feel anxious about walking or even placing their foot on the ground. The pain is likely to be more intense if you wear tight shoes, so wearing shoes that have more room in the toe area can help. Rubbing your foot may also lessen the pain.
Diagnosis
The exact cause of Mortons neuroma can often vary between patients. An accurate diagnosis must be carefully made by the podiatrist through thorough history taking and direct questioning to ensure all possible causes are addressed. The podiatrist will also gather further information about the cause through a hands on assessment where they will try to reproduce your symptoms. A biomechanical and gait analysis will also be performed to assess whether poor foot alignment and function has contributed to your neuroma.
Non Surgical Treatment
It can be helpful to perform deep stripping massage techniques along the length of the tibial nerve and the medial and lateral plantar nerves. After properly mobilizing these tissues, moving the foot and toes through a full range of motion to make sure the nerve can move freely will also be helpful. Foot pain like that occurring in Morton's neuroma, can become a debilitating and painful condition. And while massage can be helpful for this condition, it is also clear that improperly applied massage can aggravate it and make it worse. Consequently it is crucial that we use good clinical reasoning and appropriate evaluation methods to most effectively help these clients.

Surgical Treatment
If your pain continues despite several months of conservative treatment, your doctor may recommend surgery to remove the neuroma or to widen the space through which the affected nerve travels. These types of surgery often are done under local anesthesia. If your doctor removes a portion of the affected nerve along with the neuroma, you may develop permanent numbness between the toes.
Shoe Lifts The Pros Option For Leg Length Imbalances
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital means that you are born with it. One leg is structurally shorter than the other. As a result of developmental phases of aging, the brain senses the gait pattern and identifies some variation. Your body typically adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch is not really uncommon, demand Shoe Lifts to compensate and mostly does not have a profound effect over a lifetime.

Leg length inequality goes typically undiagnosed on a daily basis, however this issue is easily remedied, and can reduce many instances of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are generally affordable, frequently being below twenty dollars, in comparison to a custom orthotic of $200 or maybe more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is easily the most common condition affecting people today. Around 80 million men and women experience back pain at some point in their life. It's a problem which costs employers millions of dollars each year because of lost time and productivity. Innovative and improved treatment solutions are continually sought after in the hope of reducing the economic impact this issue causes.

People from all corners of the world suffer from foot ache due to leg length discrepancy. In these cases Shoe Lifts might be of beneficial. The lifts are capable of alleviating any discomfort in the feet. Shoe Lifts are recommended by numerous certified orthopaedic doctors.
In order to support the body in a well-balanced fashion, your feet have a vital task to play. Despite that, it can be the most overlooked zone of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts including knees, ankles and backs to be affected too. Shoe Lifts ensure that correct posture and balance are restored.

Leg length inequality goes typically undiagnosed on a daily basis, however this issue is easily remedied, and can reduce many instances of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are generally affordable, frequently being below twenty dollars, in comparison to a custom orthotic of $200 or maybe more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is easily the most common condition affecting people today. Around 80 million men and women experience back pain at some point in their life. It's a problem which costs employers millions of dollars each year because of lost time and productivity. Innovative and improved treatment solutions are continually sought after in the hope of reducing the economic impact this issue causes.

People from all corners of the world suffer from foot ache due to leg length discrepancy. In these cases Shoe Lifts might be of beneficial. The lifts are capable of alleviating any discomfort in the feet. Shoe Lifts are recommended by numerous certified orthopaedic doctors.
In order to support the body in a well-balanced fashion, your feet have a vital task to play. Despite that, it can be the most overlooked zone of the human body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts including knees, ankles and backs to be affected too. Shoe Lifts ensure that correct posture and balance are restored.
The Causes Of Calcaneal Spur

Overview
A heel spur is an overgrowth of bone that resembles a hook on the bottom of the foot. It is a reaction to stress placed on the thick connective tissue on the bottom of the foot (plantar fascia) that helps maintain the arches of the foot. Over-stress can stem from improper support of the feet. A heel spur is often accompanied by a bursitis that is a major contributor to pain.
Causes
Fctors that increase the risk of developing heel spurs include a high body mass index (BMI), regular vigorous activity, and intensive training routines or sports. Factors such as these are believed to increase the incidence of repetitive stress injuries that are associated with the formation of heel spurs. When a heel spur forms, extremely sharp pain along with the feeling that a part of the heel is trying to burst through the skin usually occurs. If left untreated, an individual may eventually begin to struggle to perform simple activities such as walking.
Symptoms
Heel spurs are most noticeable in the morning when stepping out of bed. It can be described as sharp isolated pain directly below the heel. If left untreated heel spurs can grow and become problematic long-term.
Diagnosis
Heel spurs and plantar fasciitis are diagnosed based on the history of pain and tenderness localized to these areas. They are specifically identified when there is point tenderness at the bottom of the heel, which makes it difficult to walk barefoot on tile or wood floors. X-ray examination of the foot is used to identify the bony prominence (spur) of the heel bone (calcaneus).
Non Surgical Treatment
Heel spurs are considered a self-limited condition, which means that by making small alterations in your lifestyle and regular routines you can often control the condition. The goal is to relieve pain, reduce friction and transfer pressure from your sensitive foot areas. By eliminating the cause of the heel spur and plantar fasciitis (i.e. better shoes, orthotics to fix your gait, losing weight) will help reduce the pressure put on your fascia and heel and can reduce the inflammation caused by your heel spur. Failure to see improvements after conservative treatments may make surgery your only option.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide pain relief and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. The procedure may also include removal of heel spurs.
Prevention
Walk around before you buy shoes. Before you purchase your shoes, do the following. Re-lace the shoes if you're trying on athletic shoes. Start at the farthest eyelets and apply even pressure to the laces as you come closer to the tongue of the shoe. Make sure that you can wiggle your toes freely inside of the shoe. Also, make sure that you have at enough space between your tallest toe and the end of the shoe. You should have room equal to about the width of your thumb in the tip of your shoe. Walk around to make sure that the shoe has a firm grip on your heel without sliding up and down. Walk or run a few steps to make sure your shoes are comfortable. Shoes that fit properly require no break-in period.
What Are The Signs And Symptoms Of Heel Spur

Overview
Bone spurs (retrocalcaneal spur, or exostosis) can develop not only on the back of the heel, but also on the toes, mainly around the fifth (small) toe. Most often, they occur next to the toenail on the outside of the toe; on the inside of the toe near the tip, where the fifth toe presses against the fourth toe; and on the inside of the base of the toe. Bone spurs can also occur on the sides of the toes. This is usually due to wearing shoes that are too tight in the toe box, which causes the toes to press against each other. Bone spurs may also develop in the arch area of the top of the foot; this area becomes painful when you tie your shoelaces tightly or exert other pressure on that part of the foot. Formation of spurs in this area is often associated with arthritis.
Causes
One frequent cause of heel spurs is an abnormal motion and mal-alignment of the foot called pronation. For the foot to function properly, a certain degree of pronation is required. This motion is defined as an inward action of the foot, with dropping of the inside arch as one plants the heel and advances the weight distribution to the toes during walking. When foot pronation becomes extreme from the foot turning in and dropping beyond the normal limit, a condition known as excessive pronation creates a mechanical problem in the foot. In some cases the sole or bottom of the foot flattens and becomes unstable because of this excess pronation, especially during critical times of walking and athletic activities. The portion of the plantar fascia attached into the heel bone or calcaneous begins to stretch and pull away from the heel bone.

Symptoms
Heel spurs result in a jabbing or aching sensation on or under the heel bone. The pain is often worst when you first arise in the morning and get to your feet. You may also experience pain when standing up after prolonged periods of sitting, such as work sessions at a desk or car rides. The discomfort may lessen after you spend several minutes walking, only to return later. Heel spurs can cause intermittent or chronic pain.
Diagnosis
Diagnosis of a heel spur can be done with an x-ray, which will be able to reveal the bony spur. Normally, it occurs where the plantar fascia connects to the heel bone. When the plantar fascia ligament is pulled excessively it begins to pull away from the heel bone. When this excessive pulling occurs, it causes the body to respond by depositing calcium in the injured area, resulting in the formation of the bone spur. The Plantar fascia ligament is a fibrous band of connective tissue running between the heel bone and the ball of the foot. This structure maintains the arch of the foot and distributes weight along the foot as we walk. However, due to the stress that this ligament must endure, it can easily become damaged which commonly occurs along with heel spurs.
Non Surgical Treatment
Rest your foot. Reduce the amount of weight-bearing activities you participate in. Get off of your feet and elevate them. This will allow healing to begin. Apply ice to your foot. Applications of ice packs that provide a comfortable cooling to the heel and arch (not a freezing cold) will help reduce pain, swelling, and inflammation. Apply the ice to the heel and arch (not the toes). Make sure it is comfortable, and leave on your foot for about 20 minutes, 3 times a day. If you have any medical problems such as diabetes, poor circulation, etc., discuss the use of ice with your doctor before applying the ice. Active Wrap allows you to apply comfortable cold therapy to your foot without messy ice cubes. Use while on the ?go.? Do not walk with bare feet. Always protect your heels, arches, and plantar fascia with good supportive shoes. Vionic Orthotic Flip Flops For Men and Women are designed for walking comfort with built in orthotic foot beds that help reduce foot pain from heel spurs. Use in the house or on the beach.
Surgical Treatment
Approximately 2% of people with painful heel spurs need surgery, meaning that 98 out of 100 people do well with the non-surgical treatments previously described. However, these treatments can sometimes be rather long and drawn out, and may become considerably expensive. Surgery should be considered when conservative treatment is unable to control and prevent the pain. If the pain goes away for a while, and continues to come back off and on, despite conservative treatments, surgery should be considered. If the pain really never goes away, but reaches a plateau, beyond which it does not improve despite conservative treatments, surgery should be considered. If the pain requires three or more injections of "cortisone" into the heel within a twelve month period, surgery should be considered.
Prevention
In 2002, researchers attempted to compare the effects of various running techniques on pronation and resulting injuries like stress fractures and heel spurs. They suggested that it is possible to teach runners to stride in such a way as to minimize impact forces. One way is to lower running speed. Another is to take longer rest periods following a run.